Cryptozoospermia, also known as hidden or rare sperm, is a male infertility disorder that results in a low concentration of sperm in the semen. According to a report by the National Institutes of Health on Male infertility, cryptozoospermia account for 8.73% of total male infertility factors.
Genetic diseases, pollutants and chemical exposure, hormone imbalances, infections, specific drugs, smoking, obesity, binge drinking, and other lifestyle factors may contribute to the syndrome. Low concentration of sperm impacts fertility and makes it difficult for the couple to conceive naturally.
For all the men who have been diagnosed with cryptozoospermia or have a doubt about the symptoms, consulting a fertility expert is the first and foremost step to increase the chances of conceiving a child. Assisted Reproductive Techniques (ART) like IVF, IUI, ICSI, and others can help improve overall reproductive health and may help achieve conception.
Our experts at Aastha Fertility Care have been treating infertility issues in males and females for 5+ years and understand that facts that infertility can be challenging and stressful. Hence, all our infertility experts are dedicated to providing the best infertility treatment along with emotional support, which makes a significant difference in the overall outcome of the treatments.
Let’s find out the detailed facts about cryptozoospermia to know all the ins and outs of infertility factors for easy diagnosis and conception.
Causes of Cryptozoospermia
Here are the possible causes of cryptozoospermia:
Genetic Factors
Cryptozoospermia is a disorder marked by a low sperm concentration in the semen and is primarily brought on by genetic problems. Sperm function, production, and development could be affected by Klinefelter syndrome, Y chromosomal deletions, cystic fibrosis, and other disorders. Genetic testing could pinpoint the congenital anomaly causing the illness.
Hormonal Imbalances
Interference with sperm development and production and hormonal abnormalities may develop Cryptozoospermia. Low sperm counts may be caused by pituitary, adrenal gland diseases, thyroid, luteinising hormone (LH), prolactin, oestrogen, or other elevated levels.
Life Changing Experiences with Aastha Fertility - From Doubt to Success
Drugs or nutritional supplements that alter hormone levels may also exacerbate the illness. Assisted reproductive technologies, lifestyle modifications, and dietary adjustments are all possible treatments.
Lifestyle Factors
Lifestyle can lead to decreased sperm count, with factors such as drinking alcohol, smoking, drug abuse, eating poorly, and not exercising can cause Cryptozoospermia. Environmental pollutants could impact the quality and production of sperm.
Avoiding smoking, eating well, consuming less alcohol, and exercising are lifestyle modifications that lead to increased quality and number of sperm. The illness can be avoided by limiting exposure to toxins and abstaining from performance-enhancing substances.
Environmental Factors
Cryptozoospermia, characterised by low sperm count, is brought on by environmental variable exposure like poisons, pollutants, chemicals, radiation, electromagnetic fields, and heat.
Improving sleep quality, reducing environmental pollution and poisons exposure, and regulating stress is crucial for curing or controlling the illness. Stress and sleep disorders can have a detrimental impact. The management of Cryptozoospermia has to consider environmental factors into account.
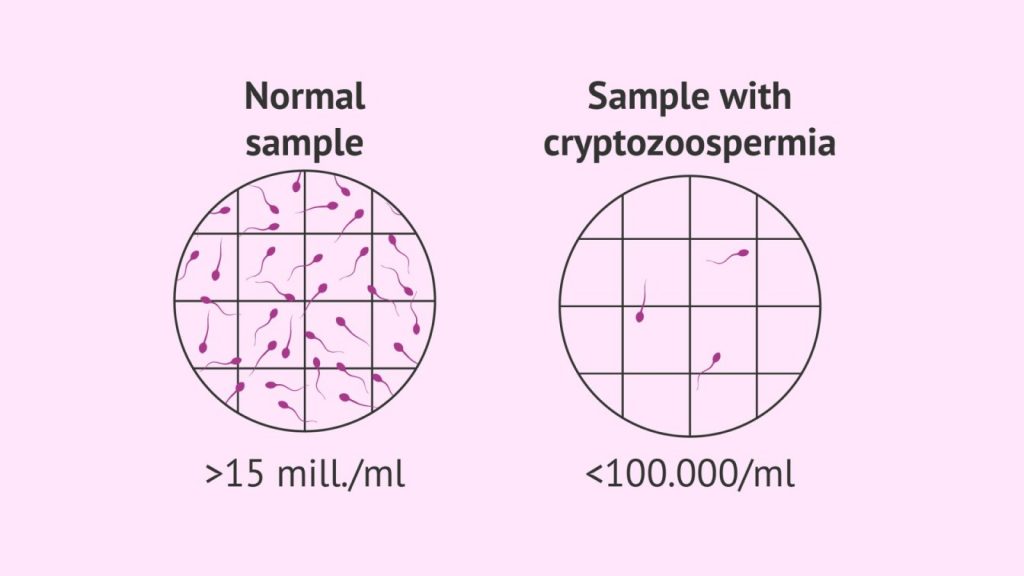
Diagnosis of Cryptozoospermia
According to the Normal sperm count report by Healthline, the average sperm count in men ranges from 15 million to more than 200 million sperm per millilitre of semen. If it drops down to less than 15 million sperm per millilitre or less than 39 million per ejaculate, then a low sperm count is diagnosed.

Semen Analysis
A semen analysis is necessary for the initial Cryptozoospermia diagnosis. A sample of sperm is taken to examine under a microscope. It evaluates the quality and number of sperm present.
Testicular Biopsy
A testicular biopsy is needed to assess if any problems are there with sperm production by examining testicular tissue. A testicular tissue sample is collected in this process and is examined in a laboratory with a microscope.
Other Diagnostic Tests
The root cause of Cryptozoospermia could be determined by additional diagnosis. The tests are done through imaging tests like ultrasound to assess the reproductive organs, genetic testing to find genetic disorders, and blood tests to assess hormone levels.
Treatment Options For Cryptozoospermia
Medical Treatments
Medical treatments help manage Cryptozoospermia and increase the likelihood of pregnancy. Gonadotropins, clomiphene citrate, human chorionic gonadotropin (hCG), and other medications may assist in improving sperm motility and sperm production. Surgical procedures are required to repair anatomical anomalies that contribute to the disorder.
Assisted Reproductive Technologies
Cryptozoospermia can be treated using assisted reproductive technologies (ARTs), including intracytoplasmic sperm injection (ICSI) and in-vitro fertilisation (IVF).
Eggs are fertilised during IVF and placed into the female’s uterus using sperm from the body’s outside. ICSI fertilises an egg by injecting one sperm right into it.
Even the most chronic Cryptozoospermia cases may respond well to such therapies. Other ART alternatives include intrauterine insemination (IUI) and intracervical insemination (ICI).
For individuals with low sperm counts, these methods can improve their odds of conceiving and assist them in achieving their goal of starting a family.
Lifestyle Changes
Cryptozoospermia can be treated well with lifestyle adjustments. Sperm quality and count could be raised by abstaining from excessive alcohol use, keeping a balanced weight, exercising regularly, avoiding smoking, controlling stress, and eating a balanced diet.
Although a lifestyle adjustment may not prove sufficient for managing chronic Cryptozoospermia cases, it might be a crucial addition to medical treatments.
Prevention and Management of Cryptozoospermia
Healthy Lifestyle Choices
To avoid and treat cryptozoospermia, one must adopt healthy lifestyle practices. It entails refraining from binge drinking, giving up tobacco use, keeping a balanced weight, working out frequently, controlling stress, and eating a balanced diet.
Avoidance of Environmental Factors
The key to managing and avoiding Cryptozoospermia is establishing healthy living practices. Avoiding environmental pollutants exposure and donning protective gear when dealing with dangerous substances is necessary.
Regular Fertility Check-Ups
For the prevention and management of cryptozoospermia, routine fertility examinations are essential. To keep track of sperm quality and count and to increase the likelihood of successful conceiving, males must regularly have their sperm analysed.
People should be urged to share their feelings honestly and seek medical attention when necessary. It’s vital to recognise that doing so is not an indication of a weak person but a solution to the problem. Various fertility services provided by Aastha Fertility Care can help treat infertility issues for both men and women.
Impact of Cryptozoospermia on Fertility
Effects On Natural Conception
- By lowering the likelihood of fertilisation because of low sperm counts, Cryptozoospermia may adversely influence conceiving naturally.
- Pregnancy primarily depends on sperm count, and the reduced number might make it challenging for sperm to fertilise an egg since the sperm’s quality is also impacted.
But, men may improve their sperm quantity and quality with the proper care, which increases the likelihood of conceiving naturally.
Effectiveness of Assisted Reproductive Technologies
- Low sperm counts caused by the disorder Cryptozoospermia may significantly affect fertility.
- In vitro fertilisation (IVF) and Intrauterine insemination (IUI) are the two options of assisted reproductive technologies (ART) that may offer an alternative.
- Achievement rates may differ based on specific characteristics like health, age, and way of living.
But the condition’s severity and the sperm’s quality affect how well ART works. For people with cryptozoospermia, ICSI with IVF or IUI with IVF is frequently the treatment choice.
Psychological Impact On Couples
- Cryptozoospermia significantly impacts the patient’s psychological health and fertility.
- Relationships may be strained due to dissatisfaction, stress, and guilt brought on by failure to get pregnant naturally.
- People dealing with emotional disturbances may benefit from counselling and support groups
Conclusion
Cryptozoospermia can significantly impact a couple’s ability to conceive, as well as their psychological well-being. Early detection and intervention are crucial, and assisted reproductive technologies (ART) can provide an opportunity for conceiving. However, success rates can be influenced by various factors such as health, lifestyle, age, disease severity, and sperm quality.
In addition to medical treatment, it is important for those experiencing psychological difficulties to seek counselling and support. At Aastha Fertility Center, Jaipur, we offer assistance and support to help individuals and couples overcome the challenges of cryptozoospermia and improve their chances of starting a family. We understand the emotional stress infertility can cause and provide a caring and compassionate environment to help our patients through this difficult time.






Leave a comment